80% of nurses say hospital care quality has deteriorated over the past two years; many nurses see vacancies remaining unfilled, increased use of travel nurses.
Four-in-ten nurses would not feel safe admitting a family member to the unit on which they work.
76% of nurses say Beacon Hill is not acting on unsafe staffing problems; Half say management does not adjust patient assignments as needed.
CANTON, Mass. – As the nation kicks off National Nurses Week (May 6 – 12) a newly released “State of Nursing in Massachusetts” survey provides a stark look at the worsening state of patient care and the lack of responsiveness by industry and state officials to nurses’ concerns about unsafe patient assignments. The 2024 edition of the annual Beacon Research survey gives the public and healthcare stakeholders a view into the current crisis through the eyes of registered nurses. In addition to the release of the survey, hundreds of the state’s RNs will be flooding the State House on May 8th at 10 a.m. to share their experiences with policy makers in the hopes of moving legislation to address the growing nursing/patient safety crisis.
- Nurses are extremely concerned about the quality of patient care in hospitals, with 80% saying care quality has gotten worse over the past two years and 49% saying it is much worse. This concern has more than doubled over the past 10 years.
- Not having enough time with patients and caring for too many patients at one time remain top challenges impeding the ability of nurses to provide quality care, with two-thirds of nurses surveyed citing each as a major challenge.
- RNs report being aware of serious negative patient outcomes as a result of understaffing, including nurses lacking time to properly comfort and assist patients and families (80% aware), nurses lacking time to educate patients and provide adequate discharge planning (76%), re-admission (65%), medical errors (55%), and even death (26%).
- Four-in-ten nurses would not feel safe admitting a family member to the unit on which they work.
- Most nurses (61%) say a lack of proper hospital regulations are contributing to unsafe patient care conditions. Yet Beacon Hill lawmakers are not responding to concerns about unsafe staffing, according to 76% of nurses.
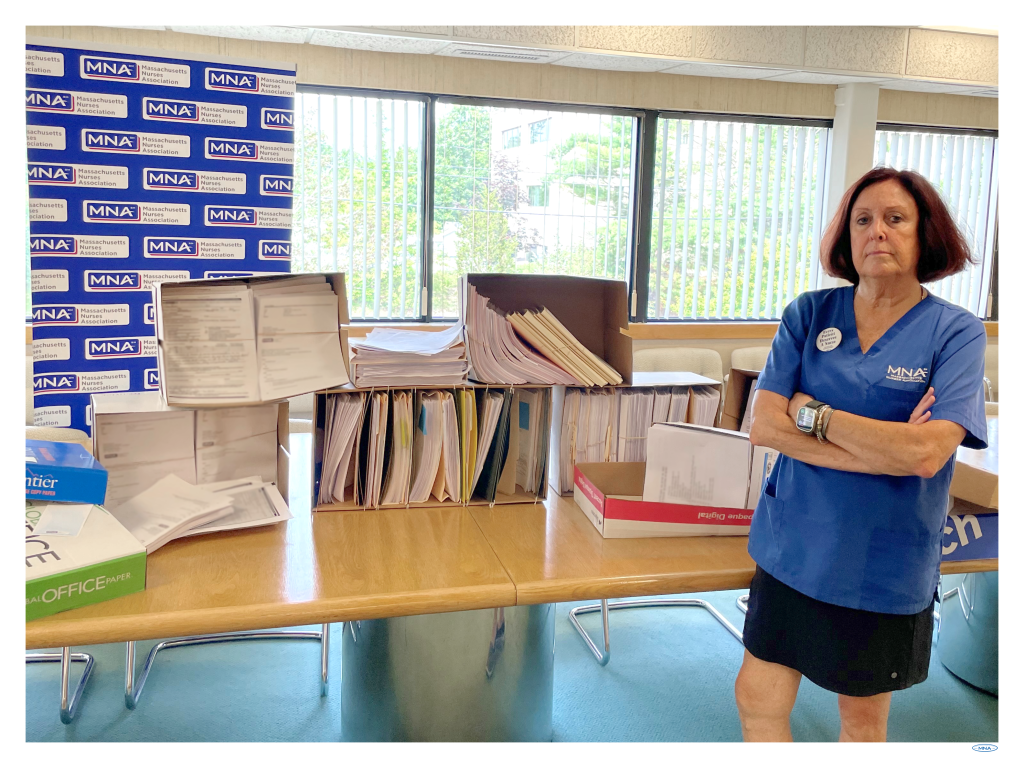
- Last year, as part of their testimony to lawmakers in favor of safe patient limits legislation, MNA nurses showed more than 12,600 unsafe staffing forms filed statewide over 18 months. These forms document instances in which nurses were forced to take an excessive patient assignment that “poses a serious threat to the safety and well-being of my patients.” Despite the enormous stack of unsafe staffing forms, lawmakers did not act.
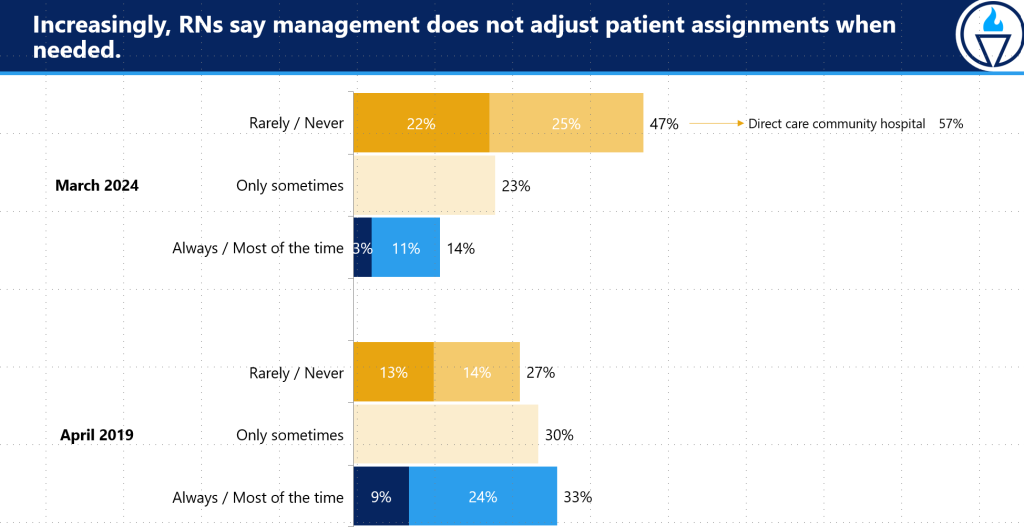
- Inside hospitals, when nurses speak up about unsafe patient assignments they are routinely ignored. 62% of nurses say administrators are not responsive to their feedback, and 47% say management rarely or never adjusts their patient loads to meet patients’ needs – up 20 points from 2019.
- For-profit owner Tenet Healthcare is an egregious example. In March, eight nurses from St. Vincent Hospital in Worcester filed a whistleblower lawsuit against Tenet. The nurses allege they were fired for exercising their legal and professional obligation to report “unsafe and illegal conduct and conditions” that jeopardized the health and dignity of the patients under their care.The lawsuit was filed around the same time the Joint Commission validated St. Vincent nurses’ concerns about patient care conditions and found the hospital to be “non-compliant with applicable Centers for Medicaid and Medicare Services (CMS) Conditions.”Nurses have spent months documenting safety concerns at the hospital. In addition to the Joint Commission, they have lodged complaints with the Department of Public Health Division of Healthcare Quality, the Center for Medicare and Medicaid Services and the Mass. Board of Registration in Nursing.
- Despite this advocacy, Tenet Healthcare refuses to acknowledge the validity of the nurses’ concerns and routinely ignores contract language safely limiting patient assignments at St. Vincent.
- Nurses do not trust their employer to keep promises and favor unionizing.
- 64% of nurses said they are dissatisfied with the influence they have in workplace decisions.
- 68% said they do not trust their employer to keep promises.
- Of the 328 non-union nurses surveyed, 56% said they would vote for a union.
- Of the 182 union nurses surveyed, 71% said they would vote to keep their union.
“The public trusts nurses and nurses trust their own ability to work together to overcome the dysfunctions of our healthcare system,” MNA President Murphy said. “The hospital industry must invest in the permanent nursing workforce. State officials must provide stronger protections for patients and nurses. Ignoring nurses’ concerns has led us to this patient care crisis. Listening to nurses is the only way to solve our problems.”
Workplace Violence a Major Concern
- Nurses experience workplace violence at extremely high rates. Yet, the survey shows employers are not taking appropriate action and are providing minimal support.
- The number of nurses who have experienced workplace violence increased 11 points from 2021, to 68% in this year’s survey.
- 30% of nurses said their employer never or rarely takes appropriate action. 22% said “sometimes.”
- 58% of nurses said they receive no additional support from their employer when they encounter violence.
Study Shows Working Conditions and Failure to Address Them is True Cause of Staffing Crisis in Massachusetts
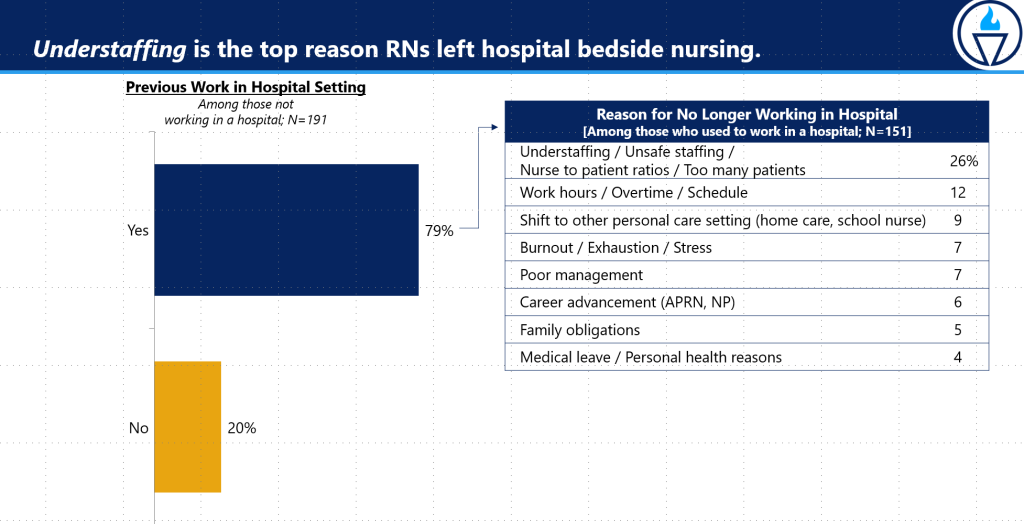
- As a result of these types of patient care conditions and the refusal of officials to listen and act, nurses are fleeing in ever greater numbers. 1 in 5 nurses plan to leave the profession within two years – twice as many as five years ago, according to “The State of Nursing in Massachusetts.” Nurses cite burnout, exhaustion, stress, and lack of employer support as major reasons for leaving.
“Nurses are clamoring for real solutions to fix the awful conditions that are driving them away from the profession and leaving patients in unsafe, overcrowded environments,” said Katie Murphy, ICU RN, and President of the Massachusetts Nurses Association. “Unfortunately, our annual survey shows that healthcare executives and state officials are failing to respond to nurses’ concerns. Instead, the industry continues to move toward temporary, remote, and app-based approaches that nurses do not like and are bad for patient care.”
- Read “The State of Nursing in Massachusetts” Executive Summary.
- See a visual representation in these survey charts.
Nurses’ Real Solutions vs. Industry’s False Answers
For “The State of Nursing in Massachusetts,” more than 500 nurses were randomly selected for interviews from the Massachusetts Board of Registration in Nursing list, including 59% who were non-union nurses. The results clearly show solutions that nurses believe will help address the crisis, as well as industry-led approaches that will make it worse.
As part of the survey – conducted between February 27 and March 11, 2024 – nurses identified significant changes in their workplace over the past two years that have contributed to unsafe staffing and deteriorating patient care conditions.
- 75% of nurses have seen RN positions left vacant or unfilled.
- 68% have seen an increase in travel nurses.
- 49% have seen an increase in the use of on-call to compensate for the lack of staff.
- 45% have seen more nurses being engaged in tasks not covered under nursing policies and procedures.
- 34% have seen an uptick in mandatory overtime.
Nurses came out plainly against app-based and remote nursing strategies in the survey.
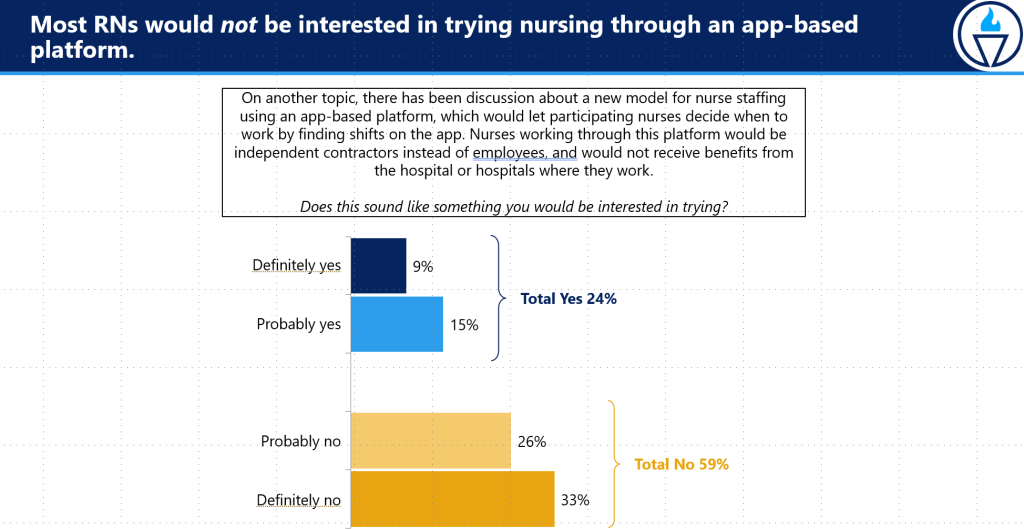
- 59% of nurses said they were not interested in using an app to work as an independent contractor without benefits.
- 61% of nurses (including 65% and 64% at direct care teaching and community hospitals) said they believe remote nursing is bad for patient care.
Instead, nurses were in favor of state and industry officials addressing the patient care crisis through safer patient assignments, investments in the permanent nurse workforce, and improved hospital regulations.
- 61% of nurses said hospitals are not properly regulated to keep patients safe.
- 54% said more regulations are needed to keep patients safe.
- 55% said salary increases could keep them from leaving the profession.
- 43% said limits on the number of patients cared for at one time could keep them from leaving.
- 37% said having additional ancillary staff could keep them from leaving.
- 33% said pension benefits could keep them from leaving.
- 29% said favorable time off benefits could keep them from leaving.
The “Shortage of Nurses” Myth
In its most recent report on the subject, “Health Care Workforce Trends and Challenges in the Era of COVID-19,” published in March 2023, the Health Policy Commission (HPC) concluded that the workforce challenges facing the healthcare system do not stem from a lack of nurses, but from an increasingly challenging work environment.
- Massachusetts has more nurses per capita than almost any other state, with 12% per capita growth since 2015.
- Unlike many other states, Massachusetts is on track to have a nursing surplus by the end of the decade.
- Massachusetts has increased the number of registered nurses by 24% – nearly 30,000 nurses over the past several years.
- The HPC also pointed out that the nursing education pipeline has remained steady.
Nurses Seek Safe Patient Limits
In overwhelming numbers, nurses support a legislative solution that would develop a statewide maximum limit on the number of patients a registered nurse at Massachusetts hospitals can be assigned at one time.
The MNA and its State House partners filed new legislation this term entitled “An Act Promoting Patient Safety and Equitable Access to Care,” sponsored by Sen. Lydia Edwards, D-Third Suffolk, and Rep. Natalie Higgins, D-4th Worcester. The bill would empower DPH to hold public stakeholder hearings and promulgate regulations that establish specific limits on the number of patients a registered nurse shall be assigned to care for at one time.
Nurses surveyed in 2023 supported the legislation by a wide margin. Seventy-six percent of all nurses said they strongly support this safe patient limits bill, and 12% somewhat support it.
Nearly every nurse (97%) surveyed with 0-5 years of experience said they “strongly support” the legislation.
“There is absolutely no question that limiting the number of patients a nurse cares for at one time is safer for patients and the only solution to the current nurse staffing crisis,” said Murphy. “The benefits of safe patient limits were settled science before the pandemic, and today there is even more research and nurse experiences to support this legislation.”
For more about the evidence behind safe patient limits, click here.
Nurses Are Under Assault, Seek Violence Prevention Legislation
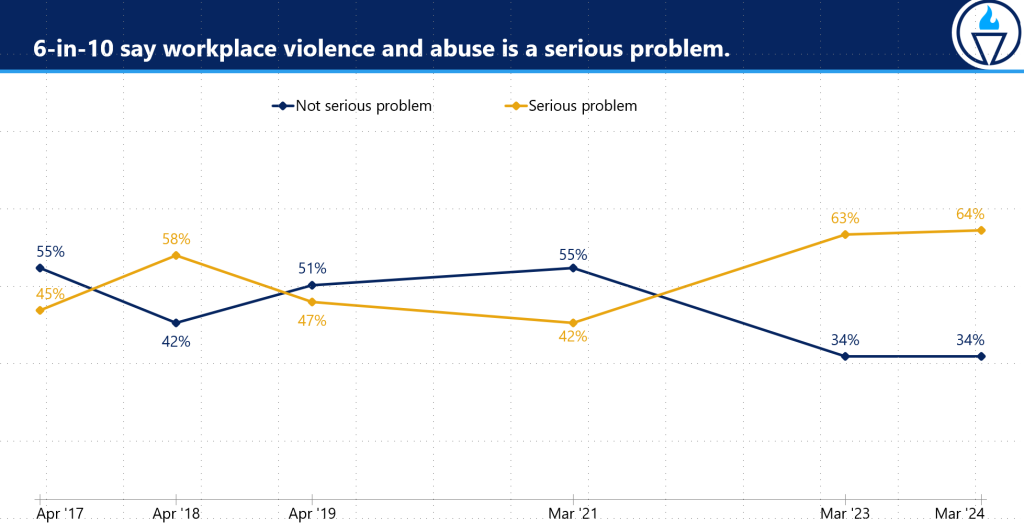
A growing number of nurses fear violence in their workplace and view it as a serious problem, according to the 2024 “State of Nursing in Massachusetts.”
Nurses have long been subject to more violence than any other profession. Nurses and nurses’ aides were assaulted more than police officers and prison guards, according to a 2017 OSHA report. To combat this worsening problem, MNA nurses and healthcare professionals have proposed violence prevention legislation at the State House.
- 64% of nurses said workplace violence is a serious problem, up 22 points from 2021.
- 68% reported experiencing at least one incident of violence in the past two years.
- Only 6% of nurses said they received paid time off in the aftermath of experiencing violence.
- Just 19% received emotional support, and 10% said they received any other kind of support from their employer.
Last legislative term, Massachusetts senators and representatives passed similar versions of the MNA bill – An Act requiring health care employers to develop and implement programs to prevent workplace violence – out of committee and to Ways and Means, the final stop before a full vote by the legislative bodies. The legislation, sponsored by Senator Joan Lovely and Representative Denise Garlick, would:
- Require healthcare employers to perform an annual safety risk assessment and, based on those findings, develop, and implement programs to minimize the danger of workplace violence to employees and patients.
- Provide time off for health care workers assaulted on the job to address legal issues.
- Allows nurses and healthcare professionals to use their health care facility address instead of their home address to handle legal issues related to an assault.
- Require semiannual reporting of assaults on health care employees to District Attorneys.
“Violence is a major contributor to burnout, is driving nurses away from the profession, and must be addressed more proactively in cooperation with staff nurses,” said Karen Coughlin, RN, and chair of the MNA Workplace Violence and Abuse Prevention Task Force. “Patients deserve nurses who feel safe at work and are fully supported by their employer.”
-###-
MassNurses.org │ Facebook.com/MassNurses │ Twitter.com/MassNurses │ Instagram.com/MassNurses
____________________________________________
Founded in 1903, the Massachusetts Nurses Association is the largest union of registered nurses in the Commonwealth of Massachusetts. Its 25,000 members advance the nursing profession by fostering high standards of nursing practice, promoting the economic and general welfare of nurses in the workplace, projecting a positive and realistic view of nursing, and by lobbying the Legislature and regulatory agencies on health care issues affecting nurses and the public.
